Real Time Eligibility
Real Time Eligibility
If you are using the calendar, we suggest use of the job scheduler. Set it up to run eligibility before the patient presents for their visit. Job Scheduler > Batch Eligibility
To review results for specific days on the calendar (if using) -Eligibility CAQ - custom appointment query
Verification is available from the:
Patient Dashboard > 'Active Policies' section, the link displays next to each insurance where real-time verification is available.
3. For Medicare / Medicaid, look to the 'other or additional payer' area
Replacement product:
- In this example under group number Blue Cross indicates this Policy is an 'Advantage' plan
- The Medicare results will list Blue Cross in the 'other or additional payer' area
- In this example, under the 'active coverage', Humana reflects 'Medicare PPO'
- The Medicare results will list Humana in the 'other or additional payer' area
\
Medicare is Secondary:Look under 'Other or Additional Payer', if there is a reason listed under 'Insurance Type Code', then Medicare is SecondaryThe user will manually add this to the Medicare Policy
How do I add eligibility request from phone calls or direct contact to the payer?
There are times a payer does not provide us with real time eligibility results. In those cases we may call or log on to the Insurance portal.
- Click the Eligibility link in the 'Active Policy' section of the patient dashboard, to review the full history of Eligibility checks and/or [ADD] manually retrieved results.

- Click [ADD] for manually retrieved results - such as a call to the Insurance or log on to their portal
- Choose which Insurance, what status
- [SAVE]
Is there a way to view historic eligibility results?
From the Patient Dashboard > in the 'Active Policy' section >' Click Eligibility'
From the Appointment screen > Click the hyperlink 'Eligibility'
- This action opens the 'Eligibility Request History' page
- Use filters for: who it was run by, when, for what DOS/Insurance, eligibility status at the time
- Click [View] to generate the full original request for review
- These requests are retained for one calendar year
From the Patient Dashboard, a ‘+’ is next to the ‘Check’ eligibility link. Click the +, a popup allows you to choose the DOS to verify Eligibility verification can also be done from the Encounter Dashboard. This will automatically verify the DOS of the Encounter.
Eligibility verification can also be done from the Encounter Dashboard. This will automatically verify the DOS of the Encounter.
 Eligibility verification can also be done from the Encounter Dashboard. This will automatically verify the DOS of the Encounter.
Eligibility verification can also be done from the Encounter Dashboard. This will automatically verify the DOS of the Encounter.
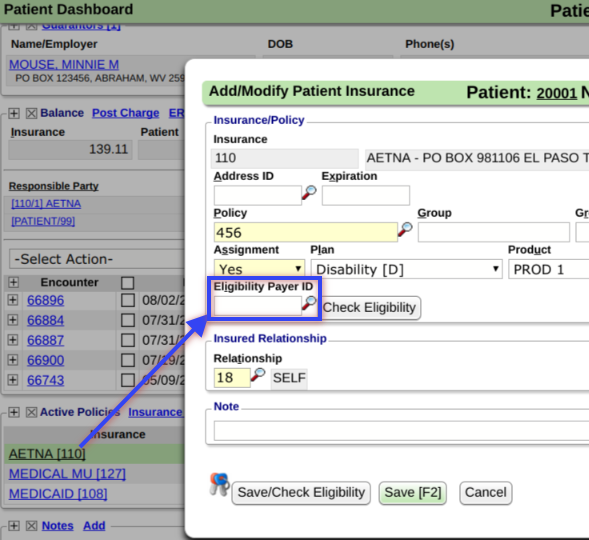
What if the Eligibility Payer ID is different than the one listed in the insurance library?
To have the system verify eligibility against a different Payer than the one designated for claims, simply add that Payer ID to this field. If the field is left blank, the system will check the Eligibility for the Payer designated in the Insurance Library.








